Friday, November 23, 2012
Cat Health News from the Winn Feline Foundation: Developing new therapies for feline mammary cancer...
Cat Health News from the Winn Feline Foundation: Developing new therapies for feline mammary cancer...: Figueira AC, Teodosio AS, Carvalheira J, Lacerda M, de Matos A and Gartner F. P-cadherin expression in feline mammary tissues. Veterinary Me...
Thursday, September 27, 2012
Monday, August 13, 2012
Please Let Me Introduce Dr. Jeremy Welsh
We are pleased to have Dr. Jeremy L. Welsh DVM MPH VPH join us on the staff of Brandywine Hospital for Pets starting July 1, 2012.
Dr. Jeremy Welsh was raised in Newcomerstown, Ohio and attended Bowling Green State University where he received his B.S. in Biology with a minor in Chemistry. Following his undergraduate degree, he relocated to Columbus, Ohio and enrolled at The Ohio State University’s College of Public Health. He graduated with honors in 2007 with a Master’s degree in Public Health specializing in Veterinary Medicine (MPH VPH). He then went on to receive his Doctor of Veterinary Medicine (DVM) at The Ohio State University’s College of Veterinary Medicine and graduated in 2011 with honors. He now resides in Zanesville, Ohio with his wife, Lisa, their two Boxers, Abraham and Lincoln and their three cats: Sebastian, Patrick, and Sebrina. Dr. Welsh enjoys spending time with his family, golfing, riding his motorcycle, gardening, traveling, and camping. Please join us in welcoming Dr. Welsh to our practice !
Tuesday, May 29, 2012
| ||||||||||
Saturday, April 14, 2012
April Is Heartworm Awareness Month
Are your pets protected against this deadly yet easily preventable disease ?
Across the country — from east to west and north to south — balmy winter weather is creating ideal conditions for an early crop of mosquitoes. And for pets, mosquitoes are more than a nuisance; these pesky little blood-sucking beasts are responsible for transmitting deadly heartworm disease.
A nationwide incidence survey conducted by the American Heartworm Society in 2010 confirmed that heartworm incidence and its risk factors are impossible to predict. Multiple variables, from microclimates to the presence of wildlife carriers, cause rates of infection to vary dramatically, even within communities. Because these factors are so variable, we never know when mosquitoes will emerge in the spring or how late into fall they’ll hang around.
Heartworm is a serious disease that threatens the lives of infected dogs and cats. Fortunately, heartworm prevention is relatively inexpensive and easy to administer. And because neither you nor your veterinarian can predict when or where your pet might be exposed, the American Heartworm Society recommends that you Think 12: (1) get your pet tested every 12 months for heartworm and (2) give your pet heartworm preventive 12 months a year.
Think 12 and you won’t need a crystal ball!
Thursday, April 5, 2012
April is Heartworm Awareness Month
Heartworm disease is a serious and potentially fatal condition caused by parasitic worms living in the arteries of the lungs and occasionally in the right side of the heart of dogs, cats and other species of mammals, including wolves, foxes, ferrets, sea lions and (in rare instances) humans. Heartworms are classified as nematodes (roundworms) and are filarids, one of many species of roundworms. Dogs and cats of any age or breed are susceptible to infection. Learn more...
Where is Heartworm Disease?
Heartworm disease has been reported in all 50 states. The map below shows particularly endemic areas based on the number of cases reported by clinics.
History
The first published description of heartworm in dogs in the United States appeared more than 100 years ago in an issue of "The Western Journal of Medicine and Surgery."1 Heartworm in cats was first described in the early 1920's.2, 3
Since then, naturally acquired heartworm infection in cats and dogs is identified as a worldwide clinical problem. Despite improved diagnostic methods, effective preventives and increasing awareness among veterinary professionals and pet owners, cases of heartworm infection continue to appear in pets around the world.
1 Osborne, TC. Worms found in the Heart and Bloodvessels of a Dog; Symptoms of Hydrophobia. The Western Journal of Medicine and Surgery, 1847.
2 Riley, WA. Dirofilaria immitis in the heart of a cat. J Parasitol 1922;9:48
3 Travassos, LP. Notas Helminthologicas. Brazil-Med. An. 1921;35 2(6):67
2 Riley, WA. Dirofilaria immitis in the heart of a cat. J Parasitol 1922;9:48
3 Travassos, LP. Notas Helminthologicas. Brazil-Med. An. 1921;35 2(6):67
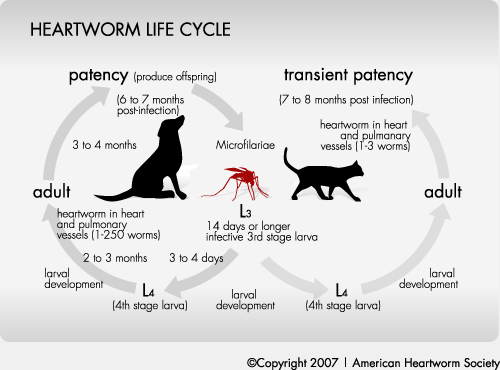
How Heartworm Happens: The Life Cycle
First, adult female heartworms release their young, called microfilariae, into an animal's bloodstream. Then, mosquitoes become infected withmicrofilariae while taking blood meal from the infected animal. During the next 10 to 14 days, the microfilariae mature to the infective larval stage within the mosquito. After that, the mosquito bites another dog, cat or other susceptible animal, and the infective larvae enter through the bite wound. It then takes a little over 6 months for the infective larvae to mature into adult worms. In dogs, the worms may live for up to 7 years. Microfilariaecannot mature into adult heartworms without first passing through a mosquito.
What Are the Signs of Heartworm Disease?
For both dogs and cats, clinical signs of heartworm disease may not be recognized in the early stages, as the number of heartworms in an animal tends to accumulate gradually over a period of months and sometimes years and after repeated mosquito bites.
Recently infected dogs may exhibit no signs of the disease, while heavily infected dogs may eventually show clinical signs, including a mild, persistent cough, reluctance to move or exercise, fatigue after only moderate exercise, reduced appetite and weight loss.
Cats may exhibit clinical signs that are very non-specific, mimicking many other feline diseases. Chronic clinical signs include vomiting, gagging, difficulty or rapid breathing, lethargy and weight loss. Signs associated with the first stage of heartworm disease, when the heartworms enter a blood vessel and are carried to the pulmonary arteries, are often mistaken for feline asthma or allergic bronchitis, when in fact they are actually due to a syndrome newly defined as Heartworm Associated Respiratory Disease (HARD).
How Do You Detect Heartworm Disease?
Heartworm infection in apparently healthy animals is usually detected with blood tests for a heartworm substance called an "antigen" ormicrofilariae, although neither test is consistently positive until about seven months after infection has occurred.
Heartworm infection may also occasionally be detected through ultrasound and/or x-ray images of the heart and lungs, although these tests are usually used in animals already known to be infected.
Prevention
Because heartworm disease is preventable, the AHS recommends that pet owners take steps now to talk to their veterinarian about how to best protect their pets from this dangerous disease. Heartworm prevention is safe, easy and inexpensive. While treatment for heartworm disease in dogs is possible, it is a complicated and expensive process, taking weeks for infected animals to recover. There is no effective treatment for heartworm disease in cats, so it is imperative that disease prevention measures be taken for cats.
There are a variety of options for preventing heartworm infection in both dogs and cats, including daily and monthly tablets and chewables, monthly topicals and a six-month injectable product available only for dogs. All of these methods are extremely effective, and when administered properly on a timely schedule, heartworm infection can be completely prevented. These medications interrupt heartworm development before adult worms reach the lungs and cause disease.
It is your responsibility to faithfully maintain the prevention program you have selected in consultation with your veterinarian.
Treatment
 Heartworms in the heart of a dog |
Usually, all but the most advanced cases of heartworm disease can be successfully treated in dogs. Currently, there are no products in the United States approved for the treatment of heartworm infection in cats. Cats have proven to be more resistant hosts to heartworm than dogs, and often appear to be able to rid themselves of infection spontaneously. Unfortunately, many cats tend to react severely to the dead worms as they are being cleared by the body, and this can result in a shock reaction, a life-threatening situation. Veterinarians will often attempt to treat an infected cat with supportive therapy measures to minimize this reaction; however it is always best to prevent the disease.
 Heartworms in the Pulmonary Artery of a dog |
Adult heartworms in dogs are killed using a drug called an adulticide that is injected into the muscle through a series of treatments. Treatment may be administered on an outpatient basis, but hospitalization is usually recommended. When the dog is sent home, exercise should be limited to leash walking for the duration of the recovery period, which can last from one to two months. This decreases the risk of partial or complete blockage of blood flow through the lungs by dead worms.
Re-infection during treatment is prevented by administration of a heartworm preventive. These preventives may also eliminate microfilariae if they are present. Dogs in heart failure and those with caval syndromerequire special attention.
Cats versus Dogs
| Cats | Dogs | |
|---|---|---|
| Parasite | Dirofilaria immitis | Dirofilaria immitis |
| Transmission | Mosquito | Mosquito |
| Susceptibility to infection | Lower than dogs - 61% to 90% of cats exposed to infective larvae become infected | Very high - virtually 100% of dogs exposed to infectivelarvae become infected |
| Longevity of worms | 2-3 years | 5-7 years |
| Ectopic infections | Not uncommon | Occasionally |
| Number of worms | Usually less than 6, 1-2 worms most common | Not uncommon to find more than 30 |
| Single-sex infections in meso- to high-endemic areas | Common | Unusual |
| Microfilaremia |
|
|
| Organ with greatest pathology | Lungs | Heart and lungs |
| Clinical importance of small worm burdens | Potentially fatal | Clinical importance depends on the size of the dog, the size of the worm burden, and exercise level |
| Diagnosis | Complex | Relatively simple |
| Treatment |
|
|
| Compounds for prevention | 4 approved in US | Several approved in US |
Wednesday, March 21, 2012
Sugar-Free Gums & Candies Can Be Dangerous For Your Dog !
Xylitol is a sugar substitute ingredient commonly found in many sugar-free gums and candies. It has also recently been added to some toothpastes. If your pet is like mine, they may like to eat any or all of these things and are therefore at risk of ingesting toxic xylitol.
Xylitol is not harmful to people but dogs metabolize it rapidly in their blood, causing their body to release insulin and quickly lower blood sugar. Signs of low blood sugar that might be noticed after ingestion are weakness, staggering, seizures, and coma. Xylitol can also lead to liver damage and death if a high enough dose is ingested. Other signs of ingestion/toxicity may include vomiting and diarrhea and these may be the first signs that are noticed.
**A TOXIC DOSE OF XYLITOL CAN BE AS LITTLE AS 1-2 PIECES OF CHEWING GUM FOR A 20 POUND DOG!!**
If you suspect your pet has ingested any amount of food or oral hygiene product containing xylitol please contact your veterinarian immediately. If the ingestion has occurred recently (within 1-2 hours) your vet may induce vomiting to eliminate as much of the xylitol from the body as possible.
Although there is not a specific antidote, blood tests can be performed to see if any changes to blood sugar or liver enzymes is occurring. Symptomatic treatment is started based on the severity of signs and may include: fluids with or without dextrose (sugar) added, anti-vomiting and anti-diarrhea medication, antibiotics, and liver protectant medication.
Remember to keep all products containing xylitol out of your pet's reach because most of them taste good to pets.
Dr. Jodi Houser
Brandywine Hospital for Pets
Xylitol toxicity in dogs - AAHA Healthypet
www.healthypet.com › Pet Care
Tuesday, March 13, 2012
Grapes and Raisins are Dangerous for Your Dog
Keep your pets away from Grapes and Raisins!Many people know that chocolate can be toxic to dogs but few are aware that something as common as grapes and raisins can be toxic and life threatening if enough are consumed. Grapes and raisins can cause acute kidney failure. Doses as low as 4 oz of grapes for a 20 pound dog can be dangerous. Raisins are more potent and as little as 1 oz of raisins for a 20 lb. dog have been shown to cause kidney failure.Clinical signs of toxicity include vomiting and lethargy which can start several hours after ingestion. Signs of acute kidney failure (not able to produce urine) can occur within 24 hours.If your pet ingests grapes or raisins, call your veterinarian or animal poison control immediately. You may be instructed to induce vomiting in your pet immediately or be instructed to bring your pet to the hospial to induce vomiting, followed by procedures to decrease absorption of the grapes/raisins into the pets system and possibly fluid therapy for a few days to support the kidneys. It is important to contact your veterinarian immediately if your pet ingests grapes or raisins as the sooner treatment is initiated, the better chance your pet has of being treated effectively.Jeff Hustey, DVM
Here are a few links for Pet Poison Hotlines
www.petpoisonhelpline.com/
www.aspca.org/pet-care/poison-control/
Friday, March 9, 2012
Lily Toxicity in Cats
 |
Lilies known to cause kidney failure in cats include the
Easter Lily, Tiger Lily, Oriental Lily, Asian Lily, Daylily, Stargazer Lily |  |
Cat owners need to know that some of the most common lily plants are highly toxic to their beloved feline companions.
Easter lilies (Lilium Iongiflorum), other species of the genus Lilium (Tiger lily, rubrum lily, Japanese show lily, Asiatic hybrid lily), some species of daylilies (Hemerocallis spp), and possibly other species of the family Liliaceae are highly toxic to cats. Ingestion can lead to kidney damage. All parts of the plant are considered toxic, and intoxication can occur with ingestion of less than one leaf. To date, the toxic component has not been determined.
Within the first two to six hours of lily ingestion, a cat might manifest intestinal upset, including vomiting, loss of appetite, and depression. Signs might temporarily subside only to return within twelve to eighteen hours as kidney damage begins. Treatment consists of rapid decontamination (inducing vomiting to remove plant material, administering activated charcoal) and intravenous fluids. Postponing treatment for more than eighteen hours can result in kidney failure and death. Therefore, prompt and aggressive veterinary care is paramount. With prompt treatment, full recovery is possible. However, if treatment is delayed, varying degrees of permanent kidney damage will occur. If the cat is not treated at all, death usually occurs in three to seven days.
Cats can be extremely inquisitive and might graze on plants in and around a house. Therefore, cat owners are encouraged to avoid placing lilies where cats reside, whether indoor or outdoor. During Easter celebration (and for that matter year-round), substituting Easter lilies and other kidney toxic plants with plants such as Easter orchids, Easter lily cactus, Easter daisy, or violets is recommended.
Sunday, February 26, 2012
|
Tuesday, February 7, 2012
February Is Pet Dental Health Month
February is Dental Health Month so let's talk teeth! Did you know that all dogs have 42 permanent teeth and cats have 30? From the smallest Chihuahua to the biggest Mastiff they all have the same number. All of their permanent teeth should erupt by 6 months and should push out the deciduous (baby) teeth. Sometimes this does not happen and the baby teeth need to be extracted. The best time to do this is during a spay or neuter procedure. Deciduous teeth that are retained can cause overcrowding and tartar buildup between the baby teeth and the permanent teeth so this is a good reason to remove them when possible. Most puppies and kittens end up swallowing their baby teeth so unfortunately they do not get to leave them under the pillow for the tooth fairy!
Stay tuned for more dental health information throughout the month.
Subscribe to:
Comments (Atom)